Alternative treatments
In addition to the effective treatments included in the PTSD Treatment Decision Aid, you may have heard of other types of treatments for PTSD. Sometimes it could be helpful to consider alternative treatments, such as when other options haven't worked or if side effects have occurred.
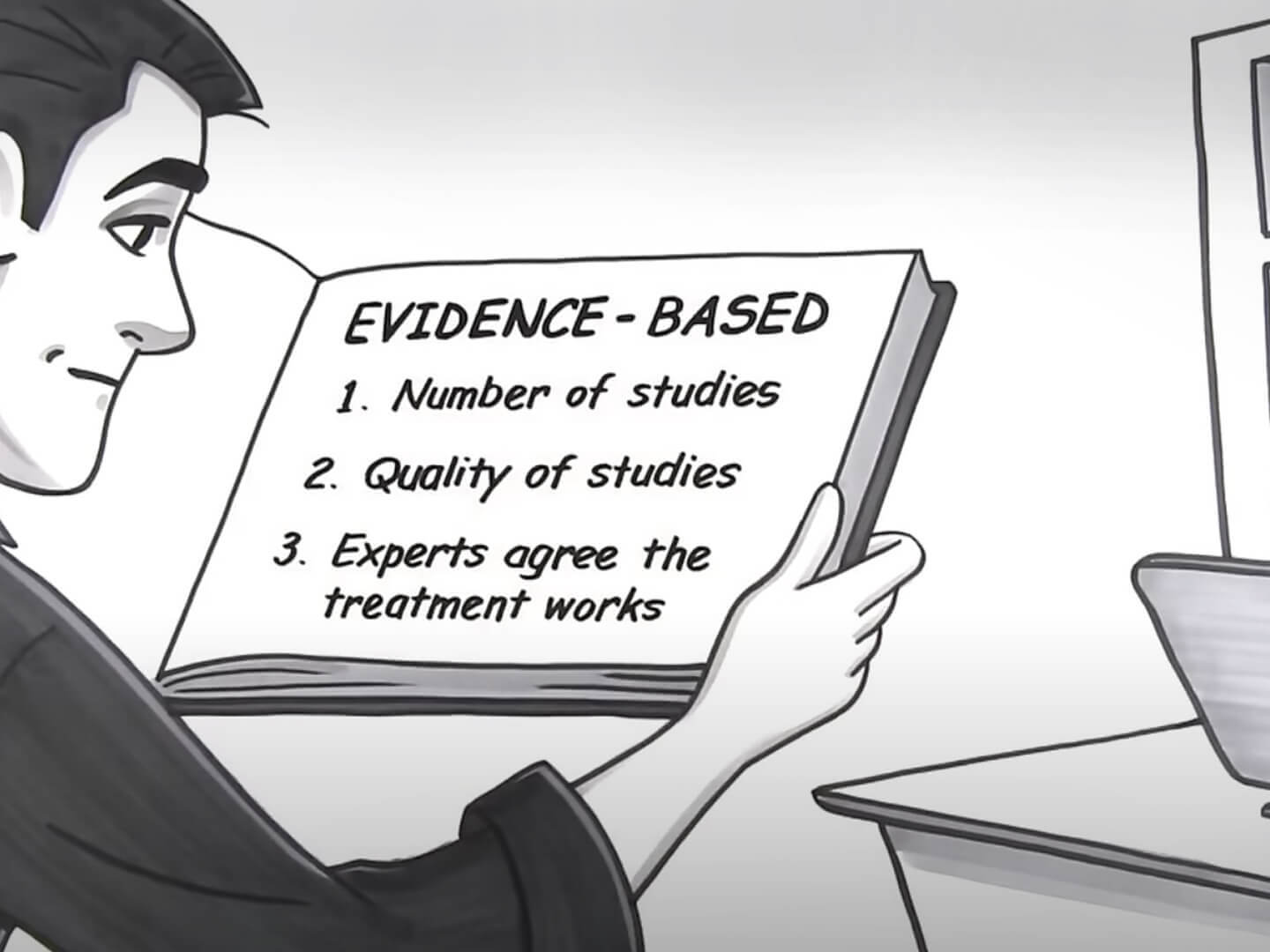
"Evidence-based" Treatment: What Does It Mean?
2:43
The list below includes other treatments that have been studied for PTSD. The evidence for these treatments is outlined according to the 2023 Clinical Practice Guideline for PTSD developed by the Department of Veterans Affairs/Department of Defense.
Some of the other treatments included in this list (e.g., meditation) may be used at the same time as any of the six treatment options discussed in the PTSD Treatment Decision Aid. You should talk with your clinician to make sure neither treatment will interfere with the other.
Other effective treatments not included in the PTSD Treatment Decision Aid
These treatments have been found to be effective but are not widely available in the United States.
Talk therapies
Cognitive Therapy for PTSD (Ehlers protocol):
a trauma-focused
cognitive-behavioral therapy that helps patients modify thoughts
and behaviors that cause the patient to feel as if they are still
under threat. The therapist helps the patient learn to modify thoughts,
then helps them revisit the trauma memory in order to develop a meaningful
account of what happened and challenge any overly negative thoughts
associated with the event. The therapist also helps the patient change any
problematic behaviors that may sustain long-term PTSD symptoms (e.g., thought
suppression).
Complementary/Integrative treatments
Mindfulness-Based Stress Reduction®:
a manualized protocol
that trains people to be aware of thoughts, sensations,
and feelings as they appear. There is also practice in being
able to not judge those thoughts and sensations. It incorporates
techniques such as mindful yoga, body scans, meditation, and
remaining mindful in daily life. Although many locations offer
some type of mindfulness, the full protocol of MBSR is not widely
available.
Not enough evidence
There is not enough scientific research to know whether these treatments are effective for PTSD. Some have not been studied very much. For others, the treatment has been studied but there is not enough information to know that the treatment works.
Medications
- 3,4-methylenedioxymethamphetamine (MDMA):
assisted psychotherapy: MDMA is a synthetic compound, also known as ecstasy, with stimulant and psychedelic properties. It likely works through altering serotonin and other neurotransmitters in the brain. It has psychological effects of increasing emotional openness, connection and empathy. MDMA-assisted psychotherapy involves having an individual take a dose of MDMA prior to undergoing a specific therapy. Other effects of MDMA use are reported to include confusion, anxiety, depression, paranoia, panic, muscle tension, cramps and teeth clenching, tremors, sweating, nausea and blurred vision. - Amitriptyline (Elavil®):
Amitriptyline is a tricyclic antidepressant (TCA) which acts by altering the levels of naturally occurring chemicals like serotonin and norepinephrine which help brain cells communicate and can lift mood. TCA side effects include constipation, blurred vision, dry mouth, drowsiness, dizziness, and changes in blood pressure. - Ayahuasca:
Ayahuasca is a plant-derived drink with psychedelic properties that can distort the senses and perception of time and alter emotional state. It is used for medicinal and spiritual reasons, primarily in South American countries. Use can be associated with hallucinations, nausea, vomiting and is possibly unsafe due to increases in heart rate and blood pressure. It likely works by altering levels of neurotransmitters such as serotonin, norepinephrine and dopamine. It is being investigated as a potential treatment for several mood, anxiety and trauma-related disorders. - Buspirone (BuSpar®):
Buspirone is an antianxiety medication. How it works is not exactly known but it is thought to relate to serotonin and dopamine receptors. Some people taking buspirone report a feeling of restlessness, dizziness, and drowsiness. - Bupropion (Wellbutrin®, Zyban®):
Bupropion affects mood by boosting levels of the neurotransmitters dopamine and norepinephrine. It is used to treat depression and nicotine addiction. Side effects include rapid heartbeat, insomnia, headache, agitation, dizziness, sweating, weight loss, dry mouth, constipation, nausea and vomiting, blurred vision, runny nose and sore throat. - Citalopram:
Citalopram is a selective serotonin reuptake inhibitor (SSRI) that affects levels of a naturally occurring chemical in the brain called serotonin. Serotonin is a neurotransmitter that plays a role in brain cell communication and influences a person's mood. Citalopram can cause both drowsiness and insomnia, sweating, nausea and dry mouth. - Desvenlafaxine (Pristiq®):
Desvenlafaxine is a serotonin norepinephrine reuptake inhibitor (SNRI) that affects levels of naturally occurring chemicals in the brain called serotonin and norepinephrine. Serotonin and norepinephrine are signaling chemicals that play a role in brain cell communication and influence a person's mood. Can cause dizziness, insomnia, sweating, nausea, dry mouth and may increase blood pressure. - Dimethyltryptamine:
DMT is the active ingredient in ayahuasca along with beta-carboline alkaloids (see above). - Duloxetine (Cymbalta®):
Duloxetine is a serotonin norepinephrine reuptake inhibitor (SNRI) that affects levels of naturally occurring chemicals in the brain called serotonin and norepinephrine. Serotonin and norepinephrine are signaling chemicals that play a role in brain cell communication and influence a person’s mood. Duloxetine is used for depression, anxiety, chronic musculoskeletal pain, diabetic nerve pain, and fibromyalgia. Side effects include headache, drowsiness, fatigue, nausea, dry mouth, abdominal pain, and muscle weakness. - Escitalopram (Lexapro®):
Escitalopram is a selective serotonin reuptake inhibitor (SSRI) that affects levels of a naturally occurring chemical in the brain called serotonin. It is used for depression and anxiety. Side effects include headache, insomnia, drowsiness, nausea, diarrhea and problems with ejaculation. - Eszopiclone (Lunesta®):
Eszopiclone is a non-benzodiazepine hypnotic which acts on the GABA receptor and causes sleepiness. It is used for insomnia and can cause abnormal thinking and behavior changes, amnesia, daytime sleepiness, and complex sleep behaviors, including sleep-walking, sleep-driving, and engaging in other activities while not fully awake. Other issues include headache and taste disturbance. In people with depression, sedatives can also worsen depression, which may include suicidal thoughts. - Ibogaine:
Ibogaine is a substance with psychedelic-like properties derived from the root bark of a central African shrub. It has been studied as a potential treatment for psychiatric conditions such as substance-use disorder, post-concussive syndrome and posttraumatic stress disorder. It likely works through modulating the serotonin and opioid systems in the brain. - Imipramine (Tofranil®):
Imipramine is a tricyclic antidepressant (TCA) which acts by increasing serotonin and norepinephrine, naturally occurring chemicals which help brain cells communicate and can lift mood. TCA side effects include constipation, blurred vision, dry mouth, drowsiness, dizziness, and changes in blood pressure. - Lamotrigine (Lamictal®):
Lamotrigine is a medication used to treat seizure disorders and some cases of bipolar disorder. It is also used for other neurological or psychiatric conditions. It is not fully known how lamotrigine works, though it may involve limiting the release of excitatory neurotransmitters in the brain. Lamotrigine can cause serious skin rashes, low blood cell counts, decreased alertness, and nausea. - Lysergic acid diethylamide:
LSD is a synthetic substance with potent psychedelic properties. LSD has been investigated as a treatment for depression, anxiety and substance use disorders. Its effects are likely due to altering levels of serotonin in the brain. LSD can alter mood, thinking and perception, shifting focus from the self to connection with others. Some experience agitation, confusion, vomiting, fear, confusion, or panic. Impairment can lead to injuries and other safety concerns. - Nefazodone (Serzone®):
Nefazodone is a serotonin reuptake inhibitor (SRI) used to treat depression that works by changing levels of serotonin and norepinephrine. Cases of life-threatening liver damage have been reported with nefazodone so monitoring for this side effect with blood tests is recommended. Other side effects include headache, drowsiness, dizziness, insomnia, agitation, dry mouth, nausea, constipation and muscle weakness. - Olanzapine (Zyprexa®):
Olanzapine is used to treat aggression, agitation, bipolar disorder, depression and schizophrenia. It works by altering several neurotransmitters: serotonin, dopamine, and histamine; and by enhancing or blocking signaling by GABA, serotonin, epinephrine and norepinephrine, and acetylcholine. Side effects can include dizziness, drowsiness, unintentional movements, restlessness, weight gain, increased appetite, dry mouth, heartburn, constipation, muscle weakness, and liver problems - Phenelzine (Nardil®):
Phenelzine is a monoamine oxidase inhibitor (MAOI) antidepressant which inactivates a naturally-occurring enzyme which breaks down the neurotransmitters serotonin, norepinephrine and dopamine. MAOIs are associated with many drug and diet interactions which can make using them challenging to use safely. - Pregabalin (Lyrica®):
Pregabalin is a medication used in numerous conditions, such as epilepsy, certain pain conditions, and some anxiety disorders. Side effects may include sleepiness, fatigue, dizziness, vision changes, dry mouth and weight gain. Pregabalin likely works by blocking release of excitatory neurotransmitters like glutamate, norephinephrine, serotonin, dopamine, substance P and others. - Psilocybin:
Psilocybin is a psychedelic substance found in certain types of mushrooms, sometimes called "magic mushrooms." Psilocybin has long been used in traditional spiritual rituals as well as recreationally and medicinally. Its effects can include distortions of the senses, altered perception of time, and "spiritual" experiences. Psilocybin is being actively investigated as a treatment for medication-resistant depression (either on its own or in combination with psychotherapy) and may have benefit in other psychiatric conditions. Research in controlled settings indicate the substance is possibly safe when taken by mouth and there is little evidence of physical dependence or withdrawal symptoms. - Quetiapine (Seroquel®):
Quetiapine is an atypical antipsychotic that acts primarily by decreasing the activity of two neurotransmitters: dopamine and serotonin. It is used to treat schizophrenia, bipolar disorder and depression. Side effects include increased appetite, weight gain, cholesterol level changes, problems with blood sugar regulation, diabetes and heart disease. It may also cause drowsiness, dizziness, agitation, headache, unintentional movements, increased blood pressure, dry mouth, and constipation. - Rivastigmine (Exelon®):
Rivastigmine is used to treat dementia, specifically Alzheimer's dementia and Parkinson disease dementia. Rivastigmine increases levels of the neurotransmitter acetylcholine in the brain. Common side effects include dizziness, headache, agitation, falls, nausea, vomiting, diarrhea, abdominal pain, tremor, decreased appetite and weight loss - Topiramate (Topamax®):
Topiramate is an anticonvulsant that is thought to decreases nerve activity by changing the flow of sodium in nerve cells and affecting activity of two opposing chemical signals, GABA and glutamate. Topiramate is used to prevent seizures and migraine headaches. It is also being tested in substance use disorders, including alcohol use disorder. Side effects include a sensation of tingling or numbness, fatigue, drowsiness, dizziness, memory problems, weight loss, abdominal pain, altered taste, nausea, diarrhea, respiratory infection, and fever.
Talk therapies
- Accelerated Resolution Therapy:
A trauma-focused therapy that helps patients to reconsolidate traumatic event memories as less emotionally laden memories. - Acceptance and Commitment Therapy:
A therapy that helps you create a meaningful life by accepting what is out of your control, clarifying what is truly important, and committing to action. - Adaptive Disclosure:
an individual therapy that helps process moral injury through imaginary conversation with a compassionate figure, apportioning blame, and making amends - Behavioral Family Therapy:
a couples therapy that provides education, communication training, anger management, and problem-solving training - Brief Eclectic Psychotherapy:
A type of trauma-focused therapy. You will practice relaxation skills, recall details of the traumatic memory, reframe negative thoughts about the trauma, write a letter about the traumatic event, and hold a farewell ritual to leave trauma in the past. - Cognitive Behavioral Conjoint Therapy:
CBCT is a trauma-focused cognitive-behavioral therapy delivered to an individual with PTSD and a loved one, most typically an intimate partner. CBCT includes psychoeducation about how PTSD symptoms influence relationship function, practice in communication and conflict management skills, exercises to promote positive affect and address avoidance, and education and practice in how to challenge trauma-related unhelpful beliefs. - Dialectical Behavior Therapy:
A therapy that teaches you skills to manage stress, regulate emotions, and improve relationships. - Emotional Freedom Techniques:
an energy therapy intervention in which a specific problem is brought to mind (either trauma or otherwise), and then the patient is directed to tap on their body in a certain sequence of locations while repeating statements of self-acceptance. - Exposure Relaxation and Rescripting Therapy (for PTSD or nightmares):
A class of trauma-nightmare-focused cognitive behavioral therapies that help a patient to change their nightmares in order to help decrease the intensity and severity of nightmares. - Group therapy:
a class of therapies taking place with multiple patients - Imagery Rehearsal Therapy (for PTSD or nightmares):
a class of trauma-nightmare-focused cognitive behavioral therapies that help a patient to change their nightmares in order to help decrease the intensity and severity of nightmares - Impact of Killing:
a therapy that helps patients explore the impact of not forgiving oneself, develop a forgiveness plan, and develop an amends plan to honor the values that were violated in the act of killing. - Interpersonal Psychotherapy:
A therapy that focuses on the impact of trauma on interpersonal relationships. - Narrative Exposure Therapy:
a trauma-focused therapy that helps patients to develop a written, chronological biography of their lives, including both traumatic and pleasant events. - Prolonged Exposure in Primary Care:
A version of Prolonged Exposure Therapy that is very brief so that it can fit into primary care appointments. - Psychodynamic therapy:
an insight-focused therapy that focuses on helping patients identify the roots of their current suffering. - Psychoeducation:
an intervention in which therapists provide patients with information about traumatic stress reactions, PTSD and other symptoms or conditions - Reconsolidation of Traumatic Memories:
a trauma-focused therapy in which the therapist helps the patient to briefly activate the trauma memory and then recall it in a specific way: the patient will imagine the trauma memory as if watching a movie in a theater, in black-and-white, and then as if watching it in rewind. - Seeking Safety:
a present-focused therapy that aims to teach patients coping skills. It is composed of 25 different topic-based modules, each associated with a safe coping skill (interpersonal, cognitive, and/or behavioral) relevant to both trauma and substance use - Stress Inoculation Training:
A cognitive-behavioral therapy that teaches skills and techniques to manage stress and reduce anxiety. - Skills Training in Affective and Interpersonal Regulation (STAIR):
A therapy focused on improving emotion regulation and interpersonal relationship skills. - Skills Training in Affective and Interpersonal Regulation in Primary Care:
a 5-session version of STAIR that focuses on improving emotion regulation and interpersonal relationship skills - Structured Approach Therapy:
a couples therapy in which the partner helps support the person with PTSD to approach feared situations and to talk about their trauma - Supportive counseling:
A unstructured therapy in which the therapist provides support, encouragement, and reassurance to help you deal with emotional distress and life problems. - Thought Field Therapy:
an energy therapy intervention in which a problem is brought to mind and and then the patient is directed to tap on their body in a certain sequence of locations to release energy blockages in the "thought field" (or energy meridian). - Trauma Informed Guilt Reduction:
a talk therapy that helps patients identify and evaluate beliefs that may contribute to guilt and shame about trauma. Then there is a focus on identifying important values and making a plan to live in line with those values - Trauma Management Therapy:
a talk therapy that involves exposure to the trauma memory and skills practice in social and emotional wellbeing - Couples Therapy:
a class of therapies that focus on increasing the wellbeing of the couple, not only the individual
Complementary/integrative treatments
- Acupuncture:
A practice that involves the insertion of thin needles through your skin at strategic points on your body to reduce pain or treat various health conditions. - Cognitively Based Compassion Training Veteran version:
a program that helps to build compassion toward oneself and others through meditation - Creative arts therapies:
using music, art, dance or other creative therapies to improve well-being. - Guided imagery:
using images to increase healing or relaxation - Hypnosis or self-hypnosis:
deliberately entering a trance—or focused attention—state and then using that state to encourage mental, emotional, or physical healing. - Loving Kindness Meditation:
a mindfulness practice that involves developing universal goodwill and positive intentions toward the self and other people - Mantram Repetition Program:
A meditation-based intervention that involves silently repeating a word or a phrase (called a "mantram"), thinking or acting intentionally, and purposefully concentrating on one thing at a time. - Mindfulness-Based Cognitive Therapy:
involves cognitive therapy to help change negative thought patterns. This is combined with mindfulness practice such as meditation and mindful breathing to help with acceptance of the present moment - Other mindfulness trainings:
(e.g., integrative exercise, Mindfulness-Based Exposure Therapy, brief mindfulness training) : all mindfulness interventions involve some focus on awareness of the present, and bringing a nonjudgmental attitude toward the self - Relaxation training:
Techniques intended to reduce stress and arousal and produce the body's relaxation response (e.g., slower breathing, lower blood pressure) - Somatic experiencing:
a body-focused therapy that aims to create awareness of inner physical sensations, seen as the carriers of the traumatic memory, so that trauma-related stress activation can be released through tolerating sensations and emotions - Tai chi or qigong:
rooted in ancient Asian traditions, involving slow-flowing intentional movements or even stationary meditation combined with breathing, awareness, and visualization. - Transcendental Meditation®:
a meditation-based intervention that involves silent repetition of a mantra - Yoga:
A practice that combines specific body postures and movements, breath control, and simple meditation.
Alternative treatments
- Recreational therapy:
uses recreation and other activities, such as Outward Bound or Adventure Rehabilitation, to improve health and wellbeing. - Aerobic or non-aerobic exercise:
using movement or physical activity to improve wellbeing. - Animal assisted therapy:
the use of animals such as dogs or horses to increase wellness. - Nature experiences:
doing activities like fishing or sailing (e.g., fishing, sailing).
Biological treatments
- Capnometry-assisted respiratory therapy:
uses a device to provide real-time feedback on breathing patterns, so that people can learn to breath in a stable pattern. - Hyperbaric Oxygen Therapy (HBOT):
A procedure that involves breathing pure oxygen in a pressurized room or chamber. - Neurofeedback:
a non-invasive treatment in which EEG or another device records brain activity, and then a computer translates that real-time neural activity into audio-visual feedback that patients can use to help them learn to self-regulate their brain activity. - NightWare© (for PTSD or nightmares):
an app that can be downloaded to an Apple watch. When a "stress threshold" is sensed, the device gives a vibration to the wrist that is meant to disrupt nightmares. - Repetitive transcranial magnetic stimulation (rTMS):
a non-invasive procedure in which magnetic fields are used to stimulate nerve cells in particular areas of the brain. - Stellate Ganglion Block (SGB):
An injection of local anesthetic into the front of the neck to reduce pain or treat various health conditions. This is also called a sympathetic block. - Transcranial Direct Current Stimulation:
a non-invasive procedure which uses electrodes on the scalp to deliver a weak direct current in order to change cortical tissue excitability.
Technology based interventions
- Mobile apps:
a variety of apps to be used on a smart phone for self-help for PTSD (such as PTSD Coach) - Self-help-based interventions:
seeking help online or in a book without guidance from a trained professional. - Facilitated internet-based cognitive behavioral:
therapy: a class of guided or facilitated app-based or self-help interventions, with brief prompting or feedback from an interventionist. There is usually much less interaction or feedback than in therapy.
Not recommended
Based on the scientific research, these treatments are not recommended for treating PTSD. Some have not been found to work in studies. Others are not recommended because they have significant risks or side effects that outweigh benefits.
Medications
- Benzodiazepines:
(e.g., alprazolam (Xanax), clonazepam (Klonopin), diazepam (Valium), lorazepam (Ativan), and temazepam (Restoril)*: Benzodiazepines are anticonvulsant medications which enhance the effect of GABA, a neurotransmitter important in regulating nerve activity and feelings of worry and fear. They provide short-term relief of anxiety and insomnia, but regular use is not recommended because of dependence, withdrawal, addiction, worse COPD and sleep apnea, lightheadedness, daytime drowsiness, fatigue, memory and speech problems, confusion, poor coordination, restlessness, falls, and accidents. Risk of worsening or new depression, irritability, and increased reports of suicide in people with panic disorder, Menstrual disorders, reduced libido, and difficulty urinating. There is risk of overdose and accidental death when benzodiazepines are combined with alcohol or strong pain medication (opioids). Examples include: alprazolam (Xanax®), clonazepam (Klonopin®), diazepam (Valium®), lorazepam (Ativan®), and temazepam (Restoril®). - Cannabis /Cannabis derivatives:
Cannabis, also called marijuana, is derived from the cannabis plant (cannabis sativa). Cannabis is sometimes prescribed to reduce nausea, improve appetite, or treat chronic pain. Common side effects include dizziness, sleepiness, vomiting, and hallucinations. Long-term side effects may include tolerance, dependence, withdrawal syndrome, psychosis, memory problems, and respiratory symptoms if smoked. - Divalproex (Depakote®):
Divalproex is an anticonvulsant that appears to work by increasing the action of the neurotransmitter GABA, which decreases nerve activity. Used for seizures, bipolar disorder, and migraine headaches. Valproate risks include serious liver, pancreas, blood cell problems. Use is not recommended in pregnant women. Other problems include abdominal pain, diarrhea, indigestion, loss of appetite, nausea, vomiting, muscle weakness, dizziness, feeling nervous, headache, insomnia, drowsiness, vision changes, tremor and hair loss. - Guanfacine (Tenex®):
Guanfacine is an antihypertensive that reduces nerve activity in the brain. It is used to treat attention deficit hyperactivity disorder (ADHD) and high blood pressure. Side effects include: abdominal pain, loss of appetite, dizziness, headache, insomnia, drowsiness and fatigue. - Ketamine (Ketalar®):
Ketamine is a general anesthetic used for surgical procedures and pain management. It is thought to block the N-methyl-D-aspartic acid (NMDA) receptor in the brain which may have a role in regulating memory and fear response. Although Ketamine is not recommended for PTSD treatment, it can be helpful in treating depression. - Prazosin (Minipres®) – except for nightmares:
Prazosin is a medication that blocks the effects of excess stress hormone (norepinephrine) in the brain. This can reduce nightmares associated with PTSD. Prazosin is also used to treat high blood pressure and prostate problems in men. It can cause dizziness, especially when starting the medication. - Risperidone (Risperdal®):
Risperidone is an atypical antipsychotic that acts primarily by decreasing the activity of two neurotransmitters: dopamine and serotonin. It is used to treat schizophrenia and bipolar disorder. Side effects include, weight gain, constipation, indigestion, excess saliva, nausea, vomiting, dry mouth, tremor and movement issues, dizziness, anxiety, headache, drowsiness, cholesterol level changes, problems with blood sugar regulation, diabetes and heart disease. - Tiagabine (Gabitril®):
Tiagabine is an anticonvulsant that appears to increase the activity of the neurotransmitter GABA. It is used to prevent seizures. Side effects include: muscle weakness, nausea, diarrhea, dizziness, feeling nervous, drowsiness, tremor and difficulty concentrating. - Vortioxetine (Trintellix®):
Vortioxetine is a selective serotonin reuptake inhibitor (SSRI) used to treat depression. It can cause diarrhea, nausea and sexual dysfunction.
Biological treatments
- Electroconvulsive Therapy (ECT):
A procedure in which electrodes are placed on the scalp and a controlled electric current is applied to cause a brief seizure in the brain. The procedure takes place while you are under general anesthesia. Although this is not recommended for PTSD, it can be very helpful in treating depression. - Vagal Nerve Stimulation (VNS):
A procedure that involves putting a device inside your body to stimulate the vagus nerve with electricity. You have a vagus nerve on each side of your body, extending from your brainstem to your abdomen.
* Important notes
- Benzodiazepines:
There is one type of treatment with considerable evidence that it does not help with PTSD symptoms, and can in fact be harmful—benzodiazepines or "benzos." Some names you may have heard for it are alprazolam (Xanax), clonazepam (Klonopin), diazepam (Valium), lorazepam (Ativan), and temazepam (Restoril). Benzos are sometimes prescribed for short-term use to treat extreme anxiety, panic, or sleep problems. In the long term, though, benzos can be addictive, cause other mental health problems, and make talk therapy less effective. If you are taking benzos for PTSD, work with your clinician when making a plan to stop. There are other treatments that are safer and more effective. - Cannabis:
Cannabis, or marijuana, is not recommended for the treatment of PTSD. There is a lack of research showing that it improves PTSD symptoms as well as research showing that it may be harmful. Multiple studies have noted the risks when using cannabis to treat PTSD, such as developing depression, anxiety, psychosis, and substance misuse.


